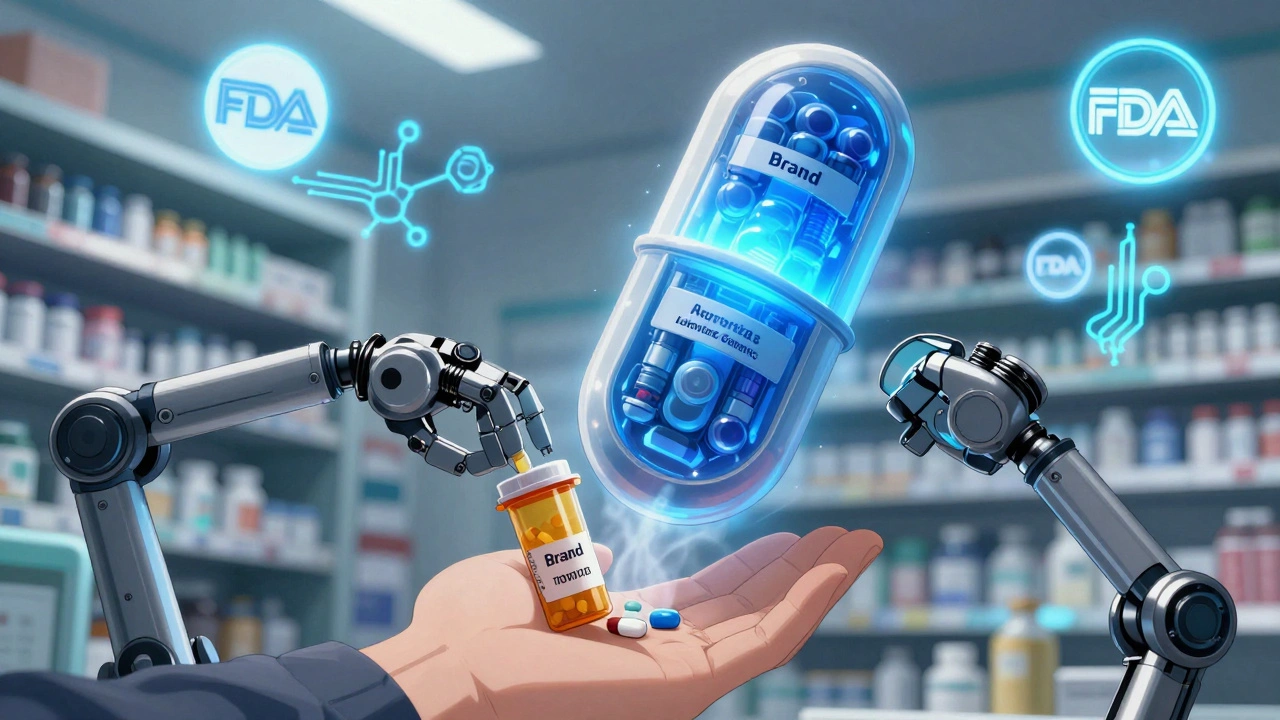
When a brand-name drug goes generic, patients often face a confusing switch. The pill looks different. The price drops. But is it the same medicine? For many, the answer isn’t clear-until they hear about authorized generics.
Authorized generics aren’t just cheaper versions. They’re the exact same drug, made by the same company that produces the brand-name version, often in the same factory, with the same active and inactive ingredients. The only difference? No brand name on the label. This makes them uniquely valuable when switching patients-especially those on medications where even tiny changes can cause problems.
Why Authorized Generics Are Different
Most generics are approved through an Abbreviated New Drug Application (ANDA). They must prove they’re bioequivalent to the brand-name drug-meaning they work the same way in the body. But they can have different fillers, dyes, or preservatives. For most people, that’s fine. For others? Not so much.
One in eight patients report side effects from inactive ingredients in regular generics. Lactose, dyes, or gluten can trigger reactions in sensitive individuals. In contrast, authorized generics share the exact same formulation as the brand. If your blood pressure medicine used to make your mouth dry with the brand, it’ll do the same with the authorized generic-because it’s the same pill, just cheaper.
The FDA confirms this: authorized generics are manufactured under the brand’s New Drug Application (NDA). No separate approval is needed. They’re not just equivalent-they’re identical.
Real Benefits for Patients
Switching to an authorized generic isn’t just about saving money-it’s about keeping treatment stable.
For patients on narrow therapeutic index drugs-like warfarin, levothyroxine, or epilepsy medications-the margin between effective and toxic doses is razor-thin. Studies show a 28% lower rate of therapeutic failure when switching to authorized generics versus regular generics. That’s not a small difference. It’s the difference between staying in control and ending up in the ER.
Switchback rates tell the story. When patients are switched to regular generics, nearly 1 in 5 return to the brand-name drug. With authorized generics? Only 7 in 100 switch back. That’s a 61% drop. For chronic conditions like asthma or heart disease, this means fewer disruptions, fewer doctor visits, and better long-term outcomes.
Patients notice it too. On patient forums and review sites, satisfaction with authorized generics hovers around 73%, compared to 58% for regular generics. Comments like, “I switched to the authorized generic of my blood thinner and haven’t had the bruising I got with the regular one,” are common. They’re not imagining it. The formulation is truly the same.
Where the System Still Fails Patients
Despite the benefits, switching to an authorized generic isn’t always smooth. Three big barriers stand in the way.
First, availability. Only about 38% of brand-name drugs with generics also have an authorized version. If your drug isn’t one of them, you can’t switch-even if you want to.
Second, insurance confusion. Some plans treat authorized generics as specialty tier drugs, even though they cost less than regular generics. One patient on Reddit shared: “My insurance covered the brand but not the authorized generic. I paid $45 more a month for the exact same pill.” That’s not a savings. That’s a penalty.
Third, lack of awareness. Nearly half of patients don’t even know authorized generics exist. Pharmacists and doctors don’t always bring them up. Patients assume all generics are the same-and end up on a version that doesn’t suit them.
Electronic health records make it worse. Over 60% of systems don’t distinguish between authorized and regular generics in medication lists. A patient’s chart might just say “lisinopril,” hiding whether they’re on the brand, a regular generic, or the authorized version. That creates risk during care transitions-like hospital discharge or pharmacy changes.
How to Manage the Transition
Switching a patient to an authorized generic doesn’t have to be a guessing game. Here’s a clear, practical five-step process:
- Check availability. Use the FDA’s Orange Book or Drugs@FDA database. Look for the phrase “Authorized Generic” next to the brand name. The FDA launched a new tool in 2023 called the “Authorized Generic Finder” to make this easier.
- Verify insurance coverage. Call the pharmacy or check the plan’s formulary. Ask: “Is the authorized generic covered at the same tier as the regular generic?” Don’t assume. Some plans charge more for authorized versions.
- Explain it clearly to the patient. Use simple language: “This is the same medicine your doctor prescribed, just without the brand name. Same ingredients. Same effects. Lower price.” Show them side-by-side images if possible.
- Coordinate with the pharmacist. Make sure the prescription is written for the authorized generic-or that the pharmacist knows to substitute it. Don’t rely on automatic substitution.
- Follow up. Check in at 14 and 30 days. Especially for high-risk drugs. Ask: “Any changes in how you feel? Any new side effects?”
For complex cases, the American Pharmacists Association recommends a 3- to 5-minute counseling session. That’s less time than you’d spend on a regular generic switch, because there’s less to explain. No need to reassure patients about bioequivalence-they’re getting the real thing.
What Experts Say
Dr. Jane Axelrad from the FDA says authorized generics offer “therapeutic consistency of brand-name products with generic pricing.” That’s the core message.
The American Medical Association’s 2023 guide recommends them specifically for patients on narrow therapeutic index drugs. Their data shows a 34% drop in adverse events when switching to authorized generics versus regular ones.
But not everyone is convinced. Some experts warn that labeling authorized generics as “better” could make patients distrust regular generics-even though FDA-approved generics are safe and effective for most. The goal isn’t to elevate one over the other, but to give patients the best option for their situation.
The Bigger Picture
The authorized generic market hit $18.7 billion in 2022. That’s 11% of all generic drug sales. And it’s growing. Analysts predict an 8.2% annual increase through 2027, driven by value-based care models that reward outcomes over cost alone.
Medicare Part D now requires plans to cover authorized generics at the same or lower cost than the brand-name drug. That’s a big win for seniors. And the FTC’s 2023 update confirmed that authorized generics still drive 5-9% retail price drops without hurting generic competition.
The FDA is also pushing for clearer labeling by 2025. That means pills and packaging will soon say “Authorized Generic” right on the label. No more confusion.

What Patients Should Ask
If you’re on a brand-name drug and it’s going generic, ask these questions:
- Is there an authorized generic version available?
- Will my insurance cover it at the same price as the regular generic?
- Will the pill look and feel the same as what I’m taking now?
- What should I watch for if I switch?
If your pharmacist or doctor doesn’t know the answer, ask them to check the FDA’s Drugs@FDA website. It’s free. It’s public. And it’s the most reliable source.
Bottom Line
Authorized generics aren’t magic. They’re just the same drug, cheaper. But for patients who need consistency-whether they have asthma, epilepsy, heart disease, or a sensitive immune system-that consistency matters more than money alone.
Switching to an authorized generic can mean fewer side effects, fewer doctor visits, and better control of your condition. But it only works if you know it’s an option-and if your system supports it.
The tools are here. The data is clear. The patients are ready. What’s missing is the conversation.
What’s the difference between an authorized generic and a regular generic?
An authorized generic is made by the same company that produces the brand-name drug, using the exact same ingredients, in the same facility. A regular generic is made by a different company and must only prove it’s bioequivalent-it can have different inactive ingredients like dyes or fillers. Authorized generics are identical to the brand; regular generics are similar.
Are authorized generics safe?
Yes. They’re not just safe-they’re the same as the brand-name drug. The FDA considers them therapeutically equivalent. The only difference is the label. They’re made under the same quality controls and inspections as the brand.
Why is my insurance charging me more for the authorized generic?
Some insurance plans incorrectly classify authorized generics as specialty-tier drugs, even though they cost less than regular generics. This is a billing error, not a policy rule. Call your insurer and ask for a formulary review. If they won’t change it, ask your pharmacist to submit a prior authorization for the authorized generic at the lower tier.
How do I know if my drug has an authorized generic?
Go to the FDA’s Drugs@FDA database and search for your brand-name drug. If an authorized generic exists, it will be listed under the “Authorized Generic” section. You can also ask your pharmacist or check the manufacturer’s website-many list authorized generics directly.
Can I switch back to the brand if I don’t feel right on the authorized generic?
If you’re on an authorized generic, switching back to the brand isn’t necessary-it’s the same drug. If you’re having issues, it’s likely due to something else: dosage, timing, or another medication. Talk to your provider before switching. If you’re on a regular generic and feel different, that’s when you should consider switching to the authorized version instead.
Are authorized generics available for all medications?
No. Only about 38% of brand-name drugs with generic alternatives have an authorized version. Availability depends on the manufacturer’s decision to produce one. Newer drugs are less likely to have them, while older, high-volume drugs like statins or blood pressure meds are more common.
Next Steps for Patients and Providers
For patients: Don’t accept a generic switch without asking if an authorized version exists. It could mean fewer side effects and better control of your condition.
For providers: Add a quick check to your prescribing workflow. When a brand goes generic, look up the authorized version. If it exists and the patient is on a narrow therapeutic index drug, make it your first recommendation.
For pharmacists: Use the FDA’s Authorized Generic Finder tool. Keep a printed list of common authorized generics in your pharmacy. Educate patients during counseling-not just about price, but about consistency.
The system isn’t perfect. But the option is real. And for the right patient, at the right time, it’s the best choice they didn’t know they had.


Jane Quitain
December 7, 2025 AT 06:57i just switched my mom to the authorized generic for her blood pressure med and she swears it feels exactly the same-no more dizziness, no weird taste. i had no idea this was even a thing until i read this. why isn’t this on every pharmacy shelf??
Ted Rosenwasser
December 8, 2025 AT 15:42Let’s be clear: the FDA’s bioequivalence standards are statistically robust and sufficient for 95% of the population. The notion that authorized generics are somehow ‘superior’ is a marketing ploy disguised as patient advocacy. Regular generics are not ‘inferior’-they’re compliant. Stop fearmongering with anecdotal reports.
Jennifer Anderson
December 9, 2025 AT 07:04my uncle’s on levothyroxine and he had crazy mood swings after switching to the regular generic-like, crying at commercials kind of stuff. we switched him to the authorized version and he’s been stable for 8 months. i wish more docs knew about this. seriously, if you’re on anything thyroid, heart, or seizure-related-ask for the authorized one. it’s not a luxury, it’s a safety net.
Oliver Damon
December 10, 2025 AT 15:43The epistemological distinction here is critical: authorized generics are ontologically identical to the branded product, whereas conventional generics are epistemically equivalent under the ANDA framework. This isn’t about ‘better’-it’s about ontological continuity. When therapeutic fidelity matters-especially with narrow TI drugs-the absence of formulation variance eliminates a latent variable in clinical outcomes. The data isn’t just suggestive; it’s statistically significant across multiple cohort studies. The real failure is systemic: EHRs don’t differentiate, formularies misclassify, and providers assume equivalence is sufficient. It’s not. It’s a logistical blind spot with clinical consequences.
Kurt Russell
December 11, 2025 AT 18:22THIS IS THE MOST IMPORTANT THING YOU’LL READ THIS YEAR. I work in a clinic and I’ve seen patients crash because they got the wrong generic. One guy had a seizure because his epilepsy med changed fillers. He didn’t know the difference. We didn’t know either-until we checked the FDA database. Now we check every switch. If your med is life-critical, don’t settle for ‘close enough.’ Get the authorized version. It’s the same pill. Just cheaper. Why are we making this hard?
Louis Llaine
December 13, 2025 AT 15:12so let me get this straight-you’re telling me i should pay extra attention to a pill that’s literally the same as the one i already take, except the label says ‘authorized generic’ instead of ‘brand name’? wow. what a revelation. next you’ll tell me water is wet.
Sam Mathew Cheriyan
December 15, 2025 AT 08:54they say authorized generics are the same but… what if the brand company is just making the generic to control the market? what if they’re secretly changing something else? i heard they use the same factory but different machines. what if the machines are calibrated differently? who really knows what’s in there? i stick with brand. they’re not lying to us… yet.
Ernie Blevins
December 16, 2025 AT 04:47so you’re telling me the drug company makes the same pill and sells it cheaper? how is that possible? they must be cutting corners. this is a scam. they’re tricking people into thinking it’s safe. i’m not dumb. i’ll stick with the brand. i’ve paid for it. i deserve it.
Nancy Carlsen
December 16, 2025 AT 06:02thank you for writing this. 🙏 i’m a nurse and i’ve seen so many patients confused about generics. i’m printing this out for my clinic. if you’re on warfarin or levothyroxine-ask for the authorized version. it’s not about being picky, it’s about being safe. you deserve to feel stable. you’re not crazy if you notice a difference. it’s real. and now you know what to ask for. 💪❤️
David Brooks
December 18, 2025 AT 04:26my wife has asthma. switched to authorized generic inhaler. no more throat irritation. no more coughing fits at night. i cried when she told me she could sleep again. this isn’t about money. it’s about dignity. if your life depends on a pill, don’t gamble with fillers. demand the real thing. even if it’s labeled ‘generic’.
Kyle Flores
December 19, 2025 AT 05:33i just learned about this and i feel kinda dumb for never asking before. my dad’s on simvastatin and he’s been having muscle pain for months. we switched to the authorized generic last week and his pain’s gone. no idea why no one ever told us this was an option. i’m gonna send this to everyone i know on meds. thanks for making it so clear. seriously, this is the kind of info that should be in every pharmacy waiting room.