Safe Travel Planner for RRMS
Travel Preparation Checklist
Click items below to mark them as completed. This checklist ensures you're fully prepared for your trip.
Insurance Comparison
Compare standard travel insurance with chronic illness coverage options.
| Feature | Travel Insurance (Chronic Add-On) | Standard Health Insurance |
|---|---|---|
| Coverage Outside Home Country | Yes, worldwide emergency care | No, only domestic |
| Pre-Existing Condition Clause | Included with stable-condition proof | Usually covered automatically |
| Medication Refill Assistance | Arranged via partner pharmacies | Handled by regular pharmacy network |
| Evacuation / Repatriation | Available for serious relapses | Rarely offered |
Emergency Plan
In Case of Relapse Abroad
- Use emergency medication as directed
- Call local emergency services
- Provide your diagnosis letter
- Head to the nearest hospital on your pre-made list
Travel Tips Summary
Medical Prep
- Carry 30-day supply of medications
- Include diagnosis letter
- Keep prescriptions handy
Accessibility
- Request wheelchair assistance
- Book accessible hotel rooms
- Select aisle seats on flights
Health Maintenance
- Stay hydrated
- Manage stress
- Control body temperature
Planning a vacation shouldn't feel like a medical exam, but living with a Relapsing‑Remitting Disease is a type of chronic illness marked by flare‑ups and periods of stability often means adding a few extra steps to the itinerary. The good news? With the right prep, you can enjoy new places, meet fresh faces, and keep your symptoms in check.
Quick Takeaways
- Gather all prescriptions, a copy of your diagnosis, and a one‑page medical summary before you leave.
- Check that your destination’s climate, altitude, and healthcare quality match your current health status.
- Purchase travel insurance that covers chronic‑illness care and pre‑authorizes hospital stays.
- Pack a portable cooling kit, mobility aids, and a hydration plan to prevent fatigue.
- Keep emergency contacts, a list of nearby hospitals, and your doctor’s contact info on your phone and in a paper copy.
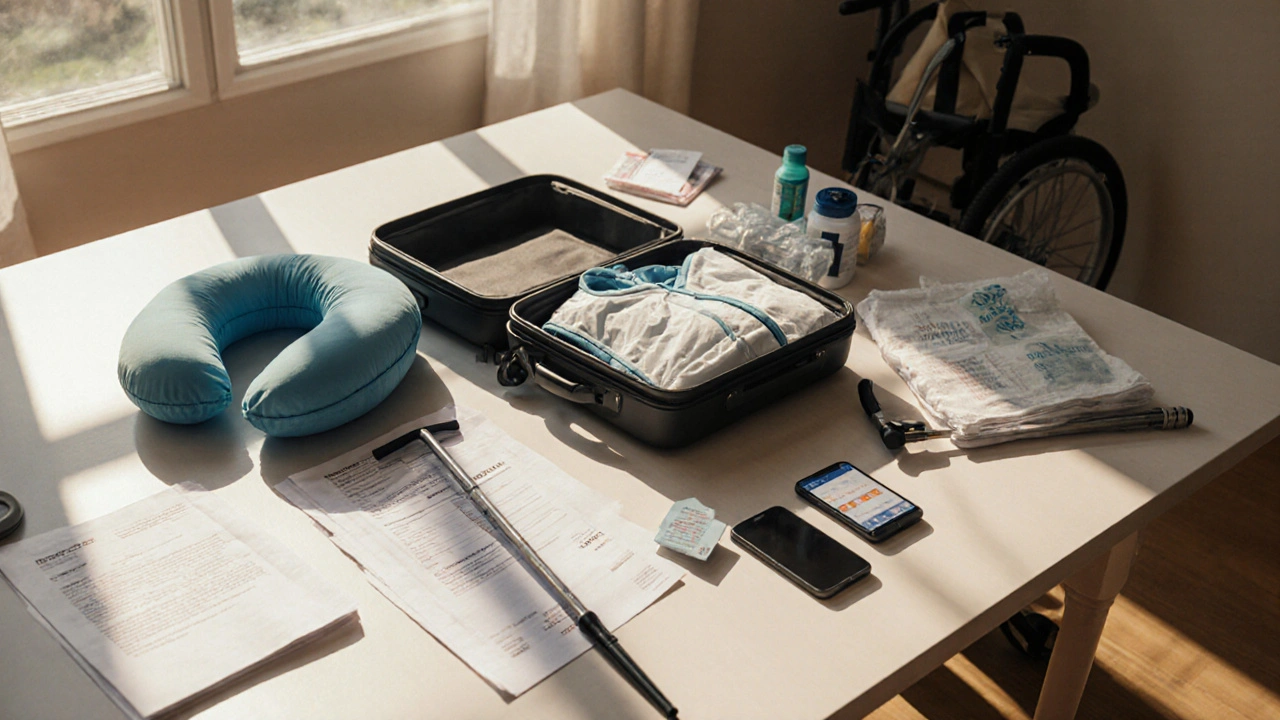
1. Build a Complete Medical Pack
Start by creating a relapsing-remitting disease travel medical pack. This isn’t just your meds; it’s a full set of documentation and tools you’ll need on the go.
- Diagnosis Letter: Ask your neurologist for a recent letter stating your condition, treatment plan, and any restrictions. Include it in both digital (PDF) and printed form.
- Medication List: Write down generic and brand names, dosages, timing, and what each drug does. Highlight any meds that require refrigeration.
- Prescription a written order for medication that can be filled at pharmacies worldwide: Carry at least a 30‑day supply plus a backup bottle in case of travel delays.
- Cooling Gear: Heat can trigger fatigue and worsen symptoms. Pack a small cooler bag, reusable ice packs, and a cooling vest if you’re heading to a hot climate.
- Mobility Aids: If you use a cane, walking stick, or portable wheelchair, bring folded versions and a spare battery for power‑assist devices.
2. Coordinate with Your Healthcare Team
Before you book a flight, schedule a tele‑visit with your Doctor the medical professional who manages your chronic condition. Use the call to:
- Confirm that your current treatment is safe for travel (especially if you’ll cross time zones).
- Get a list of approved pharmacies at your destination.
- Discuss possible flare‑up triggers like altitude or extreme temperatures.
- Ask for a short‑term steroid pack if you need emergency symptom control.
Ask the doctor to forward a copy of your medical summary to your travel insurance provider - many insurers request it for pre‑approval.
3. Choose Destination and Timing Wisely
Not all vacations are equally friendly to a relapsing‑remitting condition. Consider these factors when picking a spot:
- Climate: Extreme heat or cold can aggravate fatigue. Mid‑range temperatures (15‑25°C) are usually safest.
- Altitude: High elevations (above 2,500m) reduce oxygen levels, which may worsen neurological symptoms. If you love mountain views, stay at lower elevations and limit ascent time.
- Healthcare Access: Research nearby hospitals, neurologists, and pharmacies. Large cities typically have English‑speaking staff and 24‑hour emergency rooms.
- Travel Season: Avoid peak flu periods if you’re immunocompromised. Late spring or early autumn often offers milder weather and fewer crowds.
4. Secure the Right Insurance Coverage
Standard travel policies often exclude pre‑existing conditions. Look for a plan that explicitly covers chronic‑illness care, hospital stays, and medication refills abroad.
| Feature | Travel Insurance (Chronic‑Illness Add‑On) | Standard Health Insurance (Domestic) |
|---|---|---|
| Coverage Outside Home Country | Yes, worldwide emergency care | No, only domestic |
| Pre‑Existing Condition Clause | Included with stable‑condition proof | Usually covered automatically |
| Medication Refill Assistance | Arranged via partner pharmacies | Handled by regular pharmacy network |
| Evacuation / Repatriation | Available for serious relapses | Rarely offered |
Read the fine print: some policies require a 6‑month stable‑condition window before travel. Keep a copy of the policy and the emergency hotline in your phone.
5. Tackle Logistics and Accessibility
Airlines and hotels have become more accommodating, but you still need to ask the right questions.
- Airline Assistance: Request wheelchair support, seat near the restroom, and early boarding to settle in before the crowd pours in.
- Seat Selection: Choose an aisle seat for easy bathroom access and leg‑stretching. If you need extra legroom, consider an economy‑plus upgrade.
- Hotel Accessibility: Verify that the room has grab bars, roll‑in showers, and a ground‑floor location or elevator access.
- Local Transportation: Look for cities with low‑floor buses or wheelchair‑friendly taxis. Apps like Uber often let you select a “wheelchair‑accessible” vehicle.

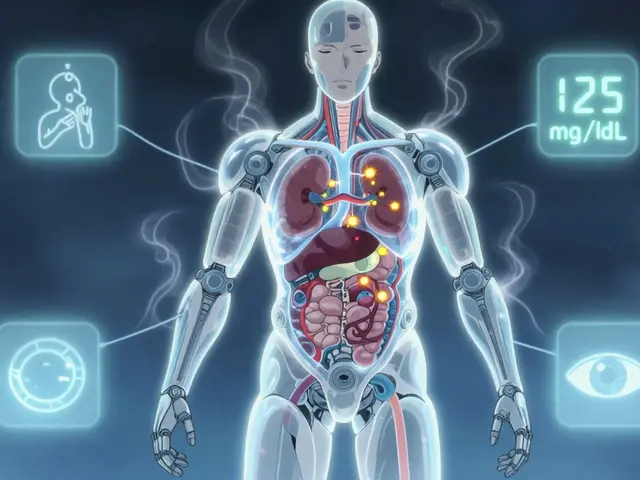
6. Keep Your Body in Balance While Traveling
Sticking to a routine helps prevent unexpected flare‑ups.
- Hydration: Aim for at least 2L of water daily. Dehydration can mimic fatigue and trigger dizziness.
- Nutrition: Pack high‑protein snacks (nuts, cheese, jerky) for times when healthy meals are scarce.
- Sleep Hygiene: Use earplugs, a travel pillow, and a blackout mask to mimic your home sleep environment.
- Stress Management: Practice deep‑breathing or a quick 5‑minute mindfulness app before long queues or flights.
- Temperature Control: Dress in layers, keep a small portable fan, and use the cooling vest during outdoor tours.
7. Have a Clear Emergency Plan
Even with meticulous prep, a relapse can happen. Being ready saves time and anxiety.
- Emergency Contact Card: Write your doctor’s name, phone, and the name of your local neurologist on a card you keep in your wallet.
- Local Hospital List: Identify the nearest hospital with an emergency department. Note the address, phone, and whether they have a neurology ward.
- Medication Access: Keep a spare set of pills in a separate bag, and know the generic names so you can request equivalents abroad.
- Travel Companion Briefing: If you’re traveling with a friend or partner, walk them through your medication schedule and what to do if you feel a new symptom.
Travel Health Checklist
| Category | Item | Notes |
|---|---|---|
| Documentation | Diagnosis letter, prescription copies, insurance card | Both digital and printed versions |
| Medications | Daily meds, backup supply, emergency steroids | Check temperature requirements |
| Cooling Gear | Portable cooler bag, reusable ice packs, cooling vest | Especially for hot destinations |
| Mobility Aids | Foldable cane, travel wheelchair, spare batteries | Pack in carry‑on |
| Health Snacks | Protein bars, nuts, dried fruit | Helps maintain energy on long travel days |
| Tech Tools | Phone with medical apps, offline maps, emergency contacts list | Backup charger and power bank |
Frequently Asked Questions
Can I bring my injectable disease‑modifying therapy on a plane?
Yes. Keep the medication in its original packaging with the prescription label. If it requires refrigeration, request a cool‑pack from the airline and store it in the overhead bin, not the cargo hold.
What should I do if I experience a sudden relapse while abroad?
First, use your emergency medication (e.g., a steroid rescue pack) as directed. Then call your local emergency number, provide your diagnosis letter, and head to the nearest hospital on your pre‑made list.
Do I need a doctor’s note for airlines to grant wheelchair assistance?
Most airlines accept a simple note stating you have limited mobility. You can request assistance online during booking or call the airline’s special‑needs desk 48hours before departure.
How can I manage time‑zone changes without disrupting my medication schedule?
Shift your dosing times gradually-about 30minutes earlier or later each day-starting a few days before travel. Use phone alarms set to the destination’s timezone once you board.
Is it safe to travel to countries with limited medical infrastructure?
Only if you have a robust contingency plan: carry extra medication, a portable cooling kit, and travel insurance that includes medical evacuation. Consider a short‑term stay in a city with better facilities before venturing into remote areas.




Taryn Thompson
October 6, 2025 AT 12:54Traveling with RRMS can feel daunting, but a solid prep plan makes a world of difference. Start by gathering all your medical documents-diagnosis letter, medication list, and prescriptions-in both digital and printed form. Pack a 30‑day supply of meds plus a backup, and don’t forget anything that needs refrigeration. Check your destination’s climate and altitude early, and flag any hotels that meet accessibility standards. Finally, verify that your travel insurance explicitly covers pre‑existing conditions and medication refills.
Lisa Lower
October 6, 2025 AT 22:37Listen up you’re not going to wing this trip you need a checklist and you need to actually tick things off as you go because half‑remembering your meds is a recipe for disaster you’ve got to have your diagnosis letter printed out and saved on your phone you also need a detailed medication schedule with dosing times and a backup supply in case your luggage gets delayed don’t forget a cooling vest if you’re heading somewhere hot and pack a portable cooler bag with ice packs for those emergencies you should also arrange wheelchair assistance with the airline at least 48 hours before departure and make sure the hotel you booked has grab bars in the bathroom and a roll‑in shower you can’t afford to assume accessibility just because the photos look nice double‑check everything in advance and you’ll thank yourself later
Dana Sellers
October 7, 2025 AT 08:21Honestly if you can’t take a few minutes to sort your meds you don’t deserve a vacation. It’s not selfish to put yourself first, the world will keep turning whether you’re there or not. Everyone should be able to travel safely, so stop making excuses and get organized now.
Damon Farnham
October 7, 2025 AT 18:04Travel, especially for those afflicted with a relapsing‑remitting condition, demands meticulous preparation; one must consider not only the logistical aspects, such as airline accommodations, but also the nuanced interplay between climate, altitude, and neuro‑inflammatory triggers; indeed, neglecting these variables is tantamount to academic negligence, which, frankly, reflects a deplorable lack of foresight.
Gary Tynes
October 8, 2025 AT 03:47Yo make sure you got all your pills in a fidget bag so you dont lose them and double check the flight for wheelchair assistance its worth the extra call early on you wont regret it
Marsha Saminathan
October 8, 2025 AT 12:07Wow that checklist is a beast, love the energy! Just a heads up add a small insulated pouch for your cooling vest, it makes a huge diff when the sun is beating down and you’re walking museums all day also grab a portable power bank for your phone meds reminder app, never know when an outlet will be free in a cafe or airport lounge and think about packing a couple of protein bars in your day bag, staying fueled helps keep fatigue at bay especially when time zones shift a lot you’re basically covering all bases now keep that momentum going
Justin Park
October 8, 2025 AT 20:27🧭 Embarking on a journey with a chronic condition is a micro‑cosm of the human quest for balance. 🌍 Every checkpoint-medication, climate, altitude-mirrors a philosophical choice: embrace uncertainty or retreat into safety. Choose wisely, and let the experience deepen your understanding of self. 🙏
Herman Rochelle
October 9, 2025 AT 04:47Great overview, the checklist really ties everything together. Keeping both digital and hard copies of your medical info is a smart move, and the emphasis on hydration can’t be overstated. I’d add that having a simple phrase in the local language for “I need medical help” can smooth communications abroad.
Stanley Platt
October 9, 2025 AT 13:07Indeed, the comprehensive approach outlined earlier aligns with best‑practice guidelines; however, one might also consider the psychological impact of travel stress on disease activity, which is often overlooked; integrating mindfulness techniques into the pre‑travel routine could further mitigate relapse risk.
Alice Settineri
October 9, 2025 AT 21:27Okay, let’s be real-if you’re not packing glittery stickers for your meds case, are you even trying? A splash of color makes the daily routine feel less like a chore and more like a party, plus it’s easier to spot if you drop it on the floor of a foreign airport.
nathaniel stewart
October 10, 2025 AT 05:47Dear traveler, I applaud your diligence in planning this expedition. It is essentail to verifiy that your insurance policy covers pre‑existing condtions, as many polcies omit this critical facet. Additionally, consider a brief consult with your neurologist to confirm that your medication schedule will remain effective across time‑zones.
Pathan Jahidkhan
October 10, 2025 AT 14:07Ah the drama of paperwork! you think a simple doc will save you from a medical nightmare but the world is full of surprises however a well‑planned itinerary can turn chaos into order
Dustin Hardage
October 10, 2025 AT 22:27When preparing for international travel with relapsing‑remitting multiple sclerosis, the most critical element is a thorough medication management strategy. Begin by requesting a comprehensive medication list from your neurologist, detailing generic names, dosages, administration times, and storage requirements. In addition, obtain a signed diagnosis letter that clearly outlines your condition, treatment plan, and any necessary accommodations; this document serves both immigration officials and foreign healthcare providers. Secure at least a 30‑day supply of each prescription, and then duplicate the entire regimen in a separate, clearly labeled container that can be carried on the aircraft. For medications that require refrigeration, acquire an FDA‑approved portable cooler with ice packs and confirm airline policies regarding the transport of cold‑chain items.
Next, evaluate your destination’s climate and altitude, as extreme temperatures and high elevation can exacerbate fatigue and spasticity. If traveling to a hot environment, prioritize cooling gear such as a wearable vest, chilled towels, and a small insulated cooler for emergency use. Conversely, in colder regions, pack thermal layers, moisture‑wicking socks, and consider a compact heating pad.
Insurance coverage must be scrutinized meticulously. Choose a plan that explicitly lists chronic‑illness coverage, medication refill assistance, and medical evacuation. Verify that the policy’s pre‑existing condition clause requires a stable‑condition window and ensure you meet that criterion before departure. Keep a digital copy of the insurance card and the emergency hotline in an accessible location on your phone.
Accessibility considerations should not be an afterthought. Contact airlines at least 48 hours prior to departure to request wheelchair assistance, a seat near the aisle, and pre‑boarding. When booking accommodations, confirm that the hotel provides roll‑in showers, grab bars, and ground‑floor access or an operational elevator.
Finally, construct a concise emergency action plan. List three nearby hospitals with neurology services, their contact numbers, and directions from your lodging. Include a brief protocol for the use of rescue steroids, noting dosage, timing, and any contraindications. Share this plan with your travel companion and rehearse the steps to ensure a swift response in case of a sudden relapse. In summary, diligent preparation across medication, climate adaptation, insurance, accessibility, and emergency planning will markedly reduce the risk of complications and empower you to enjoy a safe, fulfilling journey.
Dawson Turcott
October 11, 2025 AT 06:47Oh great, another “comprehensive guide” – because we all love reading a novel before a flight 😂 just remember you don’t have to memorise every single line, pack the stuff and go, simple as that.
Alex Jhonson
October 11, 2025 AT 15:07Hey folks, just a quick reminder to respect local customs while traveling with a health condition – a friendly smile and a polite request for accessibility can open doors that a checklist alone might not. Also, sharing a modest snack from your home country can be a great ice‑breaker and a subtle way to let others know you have specific dietary needs.
Katheryn Cochrane
October 11, 2025 AT 23:27This article reads like a corporate pamphlet, utterly devoid of genuine insight.
Michael Coakley
October 12, 2025 AT 07:47Yeah right, because “cultural ambassador” really means you’ll remember to pack the extra meds, huh?
ADETUNJI ADEPOJU
October 12, 2025 AT 16:07In the realm of travel logistics for chronic neurologic disorders, one often encounters a proliferation of procedural redundancies that, while ostensibly thorough, ultimately serve as bureaucratic noise rather than substantive facilitation.