Postherpetic Neuralgia is a chronic neuropathic pain condition that persists after the rash of shingles heals, lasting more than three months. It is characterized by burning, stabbing, or itching sensations along the affected dermatome.
When you hear the term "postherpetic neuralgia" (PHN), most people picture a lingering ache after chickenpox. The reality is more complex: PHN is a serious, often debilitating sequel of shingles, especially in older adults or those with compromised immune systems.
Why Diabetes Matters
Diabetes Mellitus is a metabolic disorder marked by chronic hyperglycemia, caused either by insufficient insulin production (type 1) or insulin resistance (type 2). High blood sugar damages small blood vessels and nerves, a process called diabetic neuropathy. This same pathway primes the nervous system for exaggerated pain responses, making diabetic patients more vulnerable to PHN.
Several mechanisms explain the link:
- Reduced immune surveillance slows the clearance of the Varicella‑Zoster Virus (VZV), the culprit behind both chickenpox and shingles, allowing the virus to reactivate more aggressively.
- Microvascular insufficiency impairs skin and nerve healing, extending the inflammatory phase after a shingles outbreak.
- Chronic inflammation associated with hyperglycemia sensitizes nociceptors, turning a mild rash into a severe, lingering pain syndrome.
Who Is at Greatest Risk?
Statistical reviews from major diabetes registries (e.g., the UK Prospective Diabetes Study) show that people with diabetes are 1.5-2times more likely to develop PHN after shingles compared to non‑diabetic peers. Age compounds the risk: patients over 60 with diabetes face a 30% cumulative incidence of PHN within a year of a shingles episode.
Key risk factors include:
- Uncontrolled Blood Sugar Control (HbA1c>8.0%).
- Long‑standing diabetes (>10years).
- Presence of peripheral neuropathy before the shingles event.
- Immunosuppressive therapy (e.g., corticosteroids).
Recognizing PHN Early
Early identification can curb severity. Watch for these red flags within the first month after shingles:
- Persistent burning or throbbing in the same dermatome.
- Allodynia - pain from light touch, such as a shirt rubbing the skin.
- Sharp, electric‑like sensations that surge with temperature changes.
If any of these linger beyond 90days, a neurologist or pain specialist should evaluate you for PHN.
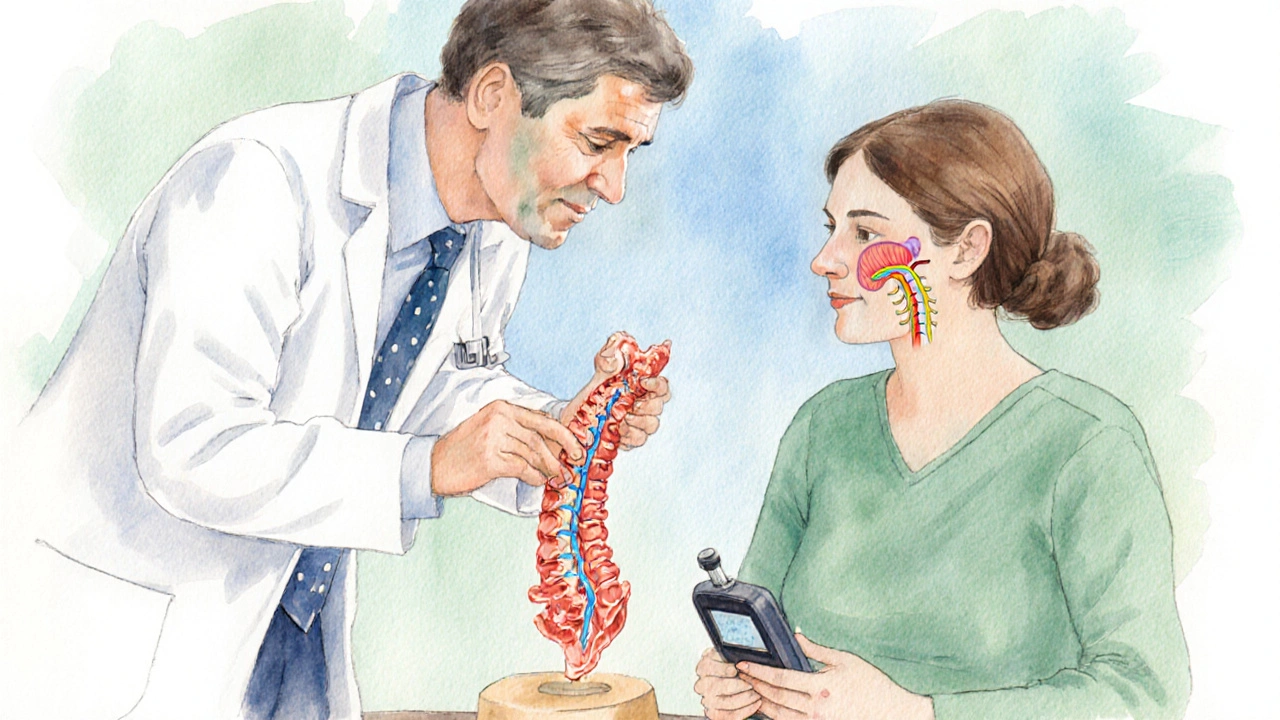
Treatment Landscape: From Antivirals to Neuropathic Drugs
Two therapeutic fronts work together: stopping the virus early and dampening the nerve pain.
Antiviral Therapy (e.g., acyclovir, valacyclovir, famciclovir) is most effective when started within 72hours of rash onset. It reduces viral replication, shortens rash duration, and modestly lowers PHN rates.
When pain persists, clinicians turn to Gabapentin, an anticonvulsant that stabilizes hyper‑excitable nerve membranes. Typical dosing for PHN starts at 300mg nightly, titrating up to 1800mg divided doses, with a 60‑% response rate in diabetic patients.
Other options include pregabalin, duloxetine, and topical lidocaine patches. Choosing the right drug depends on comorbidities, renal function, and patient preference.
Comparison of Diabetes Types and PHN Risk
| Diabetes Type | Typical Age of Onset | PHN Incidence (after shingles) | Average HbA1c in Affected Cohort | Recommended Monitoring |
|---|---|---|---|---|
| Type1 | 0-30 years | ≈12% | 8.5% | Quarterly HbA1c, annual VZV antibody check |
| Type2 | 40-70 years | ≈22% | 9.1% | Bi‑annual HbA1c, prompt antiviral if shingles appears |
The table underscores that older adults with type2 diabetes face a noticeably higher PHN burden, largely because of poorer glycemic control and age‑related immune decline.
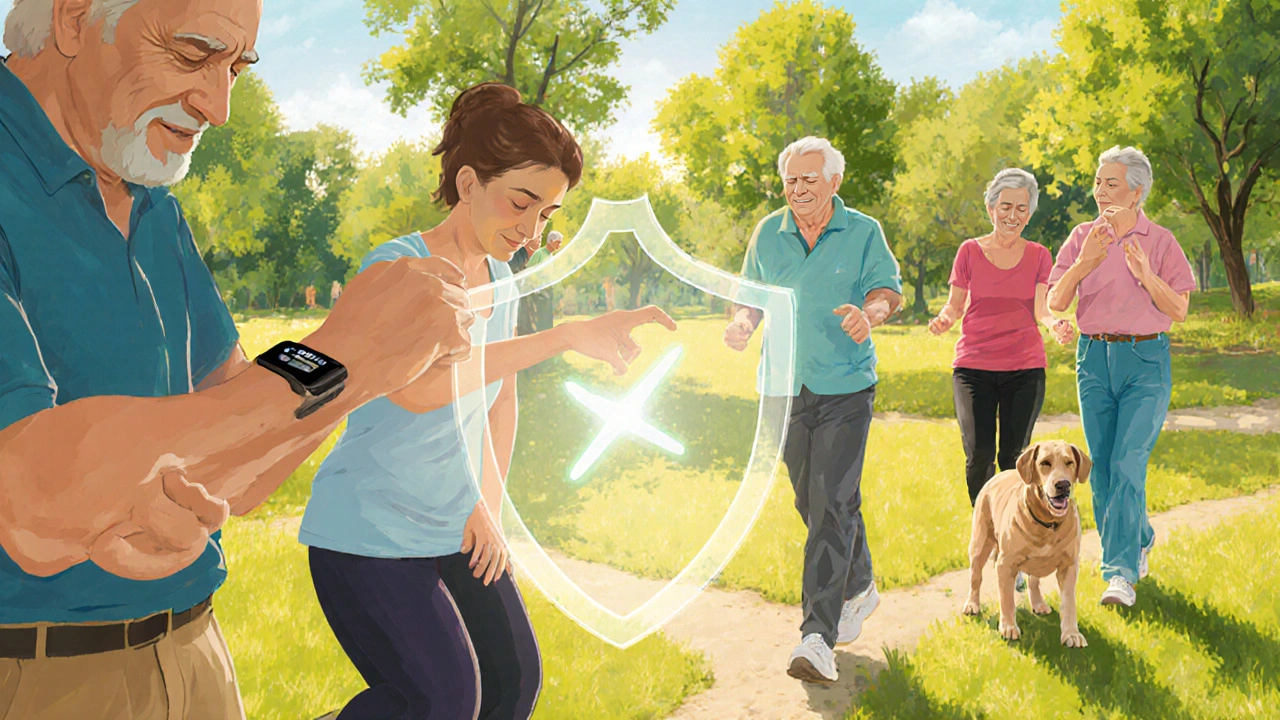
Prevention Strategies Tailored for Diabetics
Prevention is a three‑pronged approach: vaccination, meticulous glucose management, and early shingles treatment.
Vaccination - The recombinant zoster vaccine (Shingrix) has a >90% efficacy in preventing shingles and its complications, even in diabetic patients over 65. It is recommended as a two‑dose series, spaced two to six months apart.
Glycemic Control - Maintaining HbA1c below 7% reduces microvascular damage and improves immune responsiveness. Continuous glucose monitoring (CGM) helps detect excursions that could tip the balance toward neuropathy.
Rapid Antiviral Initiation - Diabetics who develop a shingles rash should see a clinician within 48hours. Oral valacyclovir 1g three times daily for seven days is the standard regimen.
Living with PHN: Daily Management Tips
Even with optimal treatment, PHN can linger. Here are practical habits that make the pain more tolerable:
- Skin care: Keep the affected area moisturized to avoid additional irritation.
- Temperature control: Warm baths can soothe burning, while cool compresses help with allodynia.
- Gentle exercise: Low‑impact activities (walking, swimming) improve circulation without over‑stimulating the nerves.
- Mind‑body techniques: Guided meditation or progressive muscle relaxation reduces central sensitization.
- Regular follow‑up: Pain scores should be reviewed every 4-6weeks to adjust medication doses.
Related Concepts and Next Steps
Understanding the diabetes‑PHN link opens doors to broader topics. You might explore:
- Diabetic peripheral neuropathy - how chronic high glucose damages nerve fibers throughout the body.
- Immunosenescence - the age‑related decline in immune function that worsens both diabetes complications and viral reactivation.
- Chronic pain pathways - the role of central sensitization in turning acute shingles pain into long‑term PHN.
Each of these areas deepens the picture of why controlling blood sugar is more than a number; it’s a shield against future nerve injuries.
Frequently Asked Questions
Does everyone with diabetes get shingles?
No. While diabetes raises the risk of VZV reactivation, most diabetics never develop shingles. Good glycemic control and vaccination dramatically lower the chance.
Can lifestyle changes reduce my PHN risk?
Yes. Maintaining stable blood sugar, staying physically active, reducing stress, and getting the shingles vaccine are proven strategies that cut down both shingles occurrence and PHN severity.
How long does PHN usually last?
The duration varies. For many, pain fades within 6-12months, but about 10% of patients experience persistent discomfort for years, especially if underlying diabetes isn’t well‑managed.
Is gabapentin safe for people with kidney problems?
Gabapentin is cleared by the kidneys, so dosage must be reduced in renal impairment. Your doctor will calculate an appropriate lower dose or suggest an alternative like duloxetine.
Should I get the shingles vaccine if I already had shingles?
Absolutely. Even after a shingles episode, the vaccine boosts immunity and lowers the chance of a second episode and subsequent PHN, which is especially important for diabetics.




Sushma Gowda
September 27, 2025 AT 20:51Great rundown on how diabetes can amplify the pain from shingles. Keeping blood sugar tight not only protects your nerves but also helps your immune system clear the virus faster. If you catch the rash early, getting antivirals within that 72‑hour window can shave off weeks of discomfort. Remember to schedule that Shingrix booster – it’s a game‑changer for anyone with chronic conditions.
Angie Wallace
October 4, 2025 AT 19:31Thanks for the reminder. I’ll talk to my doc about the vaccine soon.
Doris Montgomery
October 11, 2025 AT 18:11The article drags on with too many stats; a quick bullet list would do.
Nick Gulliver
October 18, 2025 AT 16:51Listen, the real issue isn’t just numbers – it’s that many patients ignore their meds until the pain is unbearable. Diabetes clinics should push a mandatory shingles screening at every quarterly visit. If you’re not on a glucose‑lowering plan, you’re practically inviting the virus to set up shop. The health system needs stricter protocols, not just a “maybe consider” note.
Chelsea Wilmer
October 25, 2025 AT 15:31Postherpetic neuralgia, when viewed through the lens of metabolic dysfunction, becomes a stark illustration of how systemic disease can hijack the nervous system’s resilience. The varicella‑zoster virus, dormant in dorsal root ganglia, reactivates more readily once the microvascular bed is compromised by chronic hyperglycemia, a fact underscored by the correlation between HbA1c levels and viral shedding. Moreover, the inflammatory milieu generated by advanced glycation end‑products primes nociceptors, lowering the threshold for pain and converting a benign rash into an excruciating, lingering blaze. In practice, this means that a patient with a modestly elevated HbA1c of 8.2 % is already walking a tightrope where a single shingles episode can tip them into chronic neuropathic agony. The therapeutic window, therefore, narrows dramatically; antivirals must be administered within the first three days, and analgesics should be titrated aggressively, often before the rash even resolves. Gabapentin, despite its reputation for sedation, remains the cornerstone because it targets the voltage‑gated calcium channels that are up‑regulated in diabetic nerve fibers. Yet clinicians must remain vigilant about renal dosing, especially in older adults where creatinine clearance declines. Duloxetine offers a dual benefit, addressing both mood disorders and pain modulation via serotonin‑norepinephrine reuptake inhibition, though its onset can be sluggish. Topical lidocaine patches serve as a safe adjunct, delivering localized membrane stabilization without systemic side effects. Vaccination, of course, cannot be overstated – the recombinant zoster vaccine boasts over ninety percent efficacy, even in immunocompromised cohorts, and its immunogenicity appears less blunted by hyperglycemia than the older live‑attenuated formulation. Patient education should emphasize that vaccine timing is flexible; anyone over fifty with diabetes should prioritize the two‑dose series, spacing them according to the manufacturer’s schedule. Lifestyle modifications, such as regular aerobic exercise, improve endothelial function and may indirectly bolster viral clearance mechanisms. Continuous glucose monitoring helps detect nocturnal excursions, allowing for prompt insulin adjustments that prevent sustained hyperglycemia spikes. Finally, multidisciplinary follow‑up – involving endocrinology, neurology, and pain specialists – creates a safety net that catches complications before they become intractable. The bottom line is that proactive management of diabetes does far more than preserve vision or renal function; it is a pivotal line of defense against the debilitating sequelae of shingles.
Sam Franza
October 29, 2025 AT 01:51Good points, thanks.
Raja Asif
November 3, 2025 AT 20:44Our health system should stop borrowing western protocols and enforce a strict national guideline for diabetes‑related shingles management now.
Matthew Tedder
November 6, 2025 AT 04:18I hear you; a unified protocol would indeed streamline care and reduce the waiting time for antivirals.
Cynthia Sanford
November 10, 2025 AT 19:24Sounds hopeful!
Yassin Hammachi
November 13, 2025 AT 02:58Optimism works best when paired with realistic steps – like setting a reminder for the Shingrix doses and keeping a log of blood sugar trends.
Michael Wall
November 16, 2025 AT 14:18Ignoring preventive care is simply irresponsible.
Brooks Gregoria
November 19, 2025 AT 11:44While the data looks convincing, I’d argue that the correlation between HbA1c and PHN might be overestimated due to confounding lifestyle factors. Not every diabetic who gets shingles ends up with neuralgia, and many non‑diabetics do. So, let’s not turn this into a diabetic‑only narrative. Broadening the preventive lens to include all at‑risk adults could yield a more equitable public‑health approach.
Sumit(Sirin) Vadaviya
November 23, 2025 AT 12:58Exactly! 👍 Keeping glucose stable and getting that vaccine are simple wins, and the pain relief meds are there if you need them. 😊
lindsey tran
November 25, 2025 AT 06:38Whoa, the pain can feel like tiny fireworks exploding under your skin – but don’t let it steal your sparkle! Keep fighting.
Krishna Sirdar
November 28, 2025 AT 17:58When we view health as a balance, the interplay between sugar levels and immunity becomes a natural lesson: excess tips the scales, deficiency restores it.
becca skyy
December 1, 2025 AT 15:24Totally agree, sharing these tips helps the whole community stay ahead of the curve.