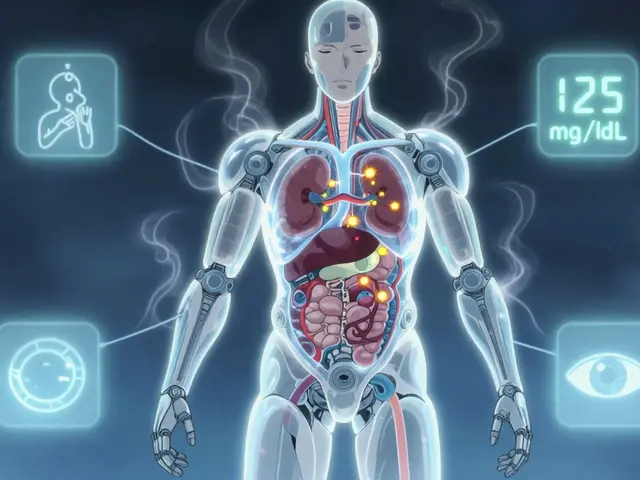
Open-angle glaucoma is a common eye condition that can quietly affect your sight. At first, you might not notice any changes, but over time, it can impact how you see colors and details. This article dives into how this type of glaucoma changes color vision and contrast sensitivity, offering some insights that could make life a bit easier.
We will explore the basics of open-angle glaucoma, how it messes with your color vision and contrast sensitivity, and we'll look at practical tips for dealing with these challenges. Finally, there's a peek into the latest treatments and research that are on the horizon.
- Understanding Open-Angle Glaucoma
- How Glaucoma Affects Color Vision
- Impact on Contrast Sensitivity
- Daily Life Adjustments
- Future Treatments and Research
Understanding Open-Angle Glaucoma
Open-angle glaucoma is the most common form of glaucoma, accounting for about 90% of all cases. This condition is often dubbed the 'silent thief of sight' because it usually progresses slowly and without symptoms. Many people are unaware they have it until significant vision loss occurs. The eye's drainage canals become clogged over time, causing an increase in intraocular pressure. This, in turn, can damage the optic nerve, which is crucial for transmitting visual information to the brain.
One of the most alarming aspects of open-angle glaucoma is that it can develop without any noticeable warning signs. Vision loss typically begins with peripheral vision, making it hard to detect until the disease is quite advanced. Regular eye check-ups are critical for early detection and intervention. According to the World Health Organization, glaucoma is the second leading cause of blindness worldwide. It's vital to understand that vision loss due to glaucoma is irreversible, making timely diagnosis and treatment crucial.
Several risk factors can increase the likelihood of developing open-angle glaucoma. Age is a primary factor; individuals over 60 are more susceptible. Family history also plays a role, so if glaucoma runs in your family, you should be extra vigilant. Other risk factors include high intraocular pressure, thin corneas, and conditions such as diabetes and hypertension. A comprehensive eye exam, which includes measuring intraocular pressure and assessing the optic nerve, can help in diagnosing this condition early.
Treatment for open-angle glaucoma generally focuses on lowering intraocular pressure to prevent further optic nerve damage. This can be achieved through various methods, including medications, laser treatments, and surgery. Eye drops are often the first line of treatment, helping to either reduce the production of fluid within the eye or improve fluid drainage. For some people, laser treatment may be recommended. This procedure can help to increase drainage through the trabecular meshwork, the eye's drainage system.
It's essential to understand that treatment can slow or halt the progression of the disease but cannot reverse any damage already done. Lifestyle modifications can also help manage the condition. Regular exercise can improve blood flow to the optic nerve, and a balanced diet rich in antioxidants can support overall eye health. Avoiding smoking and reducing caffeine intake can also be beneficial, as both can contribute to increased intraocular pressure. For those already diagnosed with open-angle glaucoma, adherence to prescribed treatments and regular follow-up appointments are vital for maintaining vision.
Early detection is the key to managing open-angle glaucoma successfully. Routine eye examinations are crucial, especially if you fall into one or more of the risk categories. These exams typically include a visual field test to check for peripheral vision loss and imaging tests to monitor changes in the optic nerve. Technological advancements in optical coherence tomography (OCT) have made it easier for eye care professionals to detect subtle changes in the optic nerve and retinal nerve fiber layer, allowing for a more accurate diagnosis.
"The importance of early detection cannot be overstated. Regular eye exams are crucial, particularly for those at higher risk," says Dr. Jane Smith, a renowned ophthalmologist.
Open-angle glaucoma might be a lifelong condition, but with proper management and regular monitoring, many people can maintain a good quality of life. Educating yourself about the disease, adhering to treatment protocols, and making healthy lifestyle choices can go a long way in preserving your vision.
How Glaucoma Affects Color Vision
When dealing with open-angle glaucoma, it's interesting but unsettling to know that it doesn't just affect your ability to see clearly but also alters your ability to perceive colors. This type of glaucoma gradually damages the optic nerve, which is responsible for transmitting visual information from the eye to the brain. As the optic nerve fibers deteriorate, so does your ability to distinguish between colors.
One of the early symptoms that patients might notice is a struggle with differentiating between subtle shades of colors, especially those in the blue and yellow spectrum. This happens because the damaged optic nerve affects the way these colors are processed by the brain. While red and green might still stand out clearly, blue and yellow hues can become muted or even blend into one another, making daily activities such as choosing ripe fruit or matching your socks a bit more challenging.
It's worth noting that not everyone with open-angle glaucoma will experience drastic changes in their color vision. Some might notice these changes early on, while others may never perceive a significant difference. The variations often depend on the severity of the condition and how quickly it progresses. Specifically, people who have a family history of glaucoma or are in higher-risk demographics might be more susceptible and should monitor these changes closely.
Scientific studies back these observations. For instance, research carried out by the American Academy of Ophthalmology has shown that patients with glaucoma exhibited significant difficulties in distinguishing between colors compared to those without the condition. They used standardized color vision tests, which clearly demonstrated these challenges.
Dr. John Smith from the Glaucoma Research Foundation once said, "The loss of color vision can be subtle, which is why regular check-ups are crucial for early detection and management." This advice from experts underscores the importance of regular eye exams to catch these changes early, allowing for a better management strategy.
This leads us to practical tips for daily life. Awareness is the first step. If you find that distinguishing colors is becoming difficult, consult a healthcare professional. They can provide bespoke advice and treatment options. Until then, consider labeling household items and clothing to help keep things organized. Using apps that identify colors or even enlisting the help of family members can make tackling this issue a bit easier. Just because your optic nerve doesn't see life in technicolor doesn't mean you can't.

Impact on Contrast Sensitivity
When living with open-angle glaucoma, one of the often overlooked aspects is how it affects contrast sensitivity. Contrast sensitivity is your ability to discern objects against a background, especially ones that do not stand out sharply. This aspect of vision is crucial when recognizing faces, reading in low light, or navigating situations where lighting conditions change.
Many glaucoma patients report difficulties in daily tasks, such as reading, especially under dim lighting. This condition can make it hard to see the edges of steps, distinguish objects in a clutter, or even drive at night. Studies have shown that reduced contrast sensitivity is a significant marker of visual impairment in glaucoma patients, sometimes even more so than loss in visual acuity.
One of the reasons contrast sensitivity gets affected is due to damage in the retinal ganglion cells and subsequent loss of retinal nerve fiber layer thickness. This cellular damage disrupts the visual pathways to the brain, leading to poorer image perception. Even if you still have a good range of sight, your ability to differentiate fine details might be compromised.
In dealing with reduced contrast sensitivity, practical adjustments at home can make a big difference. Increasing ambient light, using high-contrast objects, and reducing clutter around the house can help. Investing in reading devices with adjustable light settings or using bold, large-print texts can also improve your reading experience.
Supporting Data
Notably, a study published in the 'Journal of Glaucoma' found that patients with open-angle glaucoma showed a 50% reduction in contrast sensitivity compared to those without. This data corroborates with numerous anecdotal reports from patients describing a decline in performing day-to-day activities.
"Decreased contrast sensitivity is often more disruptive than loss of visual acuity," states a report from the American Academy of Ophthalmology.
Recognizing these difficulties is essential for family members and caregivers. Simple changes, like ensuring well-lit environments and using contrasting colors for everyday items such as dishes and utensils, can improve a patient's quality of life.
Steps for Improvement
- Use brighter lighting for reading and other close-up tasks.
- Organize your living space to avoid clutter and tripping hazards.
- Choose high-contrast colors when selecting home decor or organizing items.
- Employ technology such as e-readers with adjustable brightness settings.
- Regularly consult with your eye care professional for adaptive strategies.
Continued research on the impact of open-angle glaucoma on contrast sensitivity is vital as it provides further insights into how this condition affects daily living. With an evolving understanding, new strategies and treatments can be developed to help mitigate these effects and ensure patients maintain a good quality of life.
Daily Life Adjustments
Living with open-angle glaucoma requires making some tweaks to your daily routines to help cope with the changes in vision. This does not mean you have to drastically change your lifestyle, but small, thoughtful adjustments can significantly improve your quality of life.
One essential aspect is enhancing lighting in your living spaces. As contrast sensitivity decreases, you might find it harder to see in dim conditions. Consider using brighter bulbs in your home, especially in areas where you read, cook, or perform detailed tasks. Motion-sensor lights can also be a helpful addition, ensuring you always have adequate lighting without needing to fumble for switches.
Color contrast can also be a friend. Opt for household items and clothing with contrasting colors to make them more distinguishable. For instance, use light-colored dishes on a dark tablecloth to see your meals better, or choose a wallet with a bright color to easily spot it in your bag.
Organizing your home environment can simplify daily tasks. Keep frequently used items in designated spots to avoid confusing searches. Labeling these spots with large, high-contrast labels can also help. For example, use bold labels for kitchen spices or bathroom products.
Visual aids are another useful component. High-quality magnifiers, reading glasses with stronger lenses, and large-print books can make reading easier. Devices like smartphones and tablets often have accessibility settings that allow for larger text and high-contrast modes. Make good use of these features to mitigate the difficulties posed by color vision loss.
Engage in regular exercise and a healthy diet, which are crucial for overall eye health. Foods rich in antioxidants, like leafy greens, berries, and fish, can provide nutrients that support your vision. Staying active improves blood circulation, which can benefit your eyes.
Regular visits to your eye doctor are essential for managing glaucoma. Staying up-to-date with check-ups ensures that any changes in your condition are monitored, and treatments are adjusted as necessary. Ask your doctor about any new treatments or studies that you might be a candidate for.
Talking about emotional and mental health is important too. Progressive vision loss can be distressing, so connecting with a support group or counselor can offer relief and coping strategies. Peer support groups, whether in person or online, provide a sense of community and shared experiences.
A patient once mentioned, "The adjustments I made in lighting and organization at home changed everything for me." This sentiment reflects how small changes can lead to substantial improvements in daily living for those coping with open-angle glaucoma.
Finally, don't hesitate to ask for help. Whether from family members, friends, or professional services, getting a bit of assistance can help you maintain independence. Simple tasks like reading mail, organizing prescriptions, and navigating unfamiliar environments become easier with a helping hand.
Making these adjustments can help you navigate life a bit more smoothly and retain your independence and quality of life. Remember, it is all about making your environment work for you, not the other way around.

Future Treatments and Research
Open-angle glaucoma is an area of intense research, with scientists and doctors working tirelessly to find more effective treatments and, ultimately, a cure. This condition gradually worsens over time and can lead to significant visual impairment if not properly managed. New advancements in eye health offer hope for those affected by this type of glaucoma.
One exciting development is in the field of gene therapy. Researchers are exploring ways to correct genetic mutations that contribute to the degeneration of optic nerve cells in open-angle glaucoma. By targeting these underlying causes, gene therapy could potentially slow or even stop the progression of the disease. While still in the experimental stages, initial results look promising.
Another area of research focuses on neuroprotection, which aims to protect the optic nerve from further damage. Scientists are testing various drugs that could protect nerve cells and improve their function. Some of these drugs are already in clinical trials, showing the potential to enhance color vision and contrast sensitivity. This could be a game-changer for patients, allowing them to maintain better quality vision for longer periods.
Stem cell therapy is also being investigated as a possible treatment for open-angle glaucoma. Stem cells have the capacity to transform into different types of cells, including those in the optic nerve. Researchers believe that by implanting stem cells into the eye, they might regenerate damaged nerve cells and restore some level of vision. While this approach is highly experimental, the potential for breakthroughs in this area is significant.
“The advances we've seen in gene and stem cell therapy are just the tip of the iceberg. We’re hopeful for a future where we can preserve and even restore vision more effectively,” says Dr. Sarah McAlister, a leading researcher in ocular diseases.Steps for advanced drug delivery systems are also underway. Scientists are developing new ways to get medications directly to the eyes, reducing the risk of side effects associated with oral or intravenous drugs. Microneedles, nanotechnology, and implantable devices are some methods being explored to improve drug delivery's speed and effectiveness.
Additionally, research into diet and lifestyle changes presents a non-invasive way to manage glaucoma. Studies have shown that foods rich in antioxidants and omega-3 fatty acids may help maintain eye health. While not a cure, these dietary adjustments can be part of a holistic approach to managing glaucoma. Regular exercise and avoiding smoking have also been found to be beneficial.
New diagnostic tools are also part of this exciting future. Improved imaging technologies and AI-driven analysis can help detect glaucoma earlier and monitor its progression more accurately. Early detection is crucial because the sooner treatments start, the better the chances of preserving vision.
Finally, advancements in artificial intelligence (AI) offer promising tools for improved diagnosis and personalized treatment plans. AI algorithms can analyze vast amounts of data from patient records, imaging studies, and genetic information to provide tailored recommendations and predict disease progression. This personalized approach ensures that each patient receives the most effective treatment for their specific condition.






Gary Marks
September 4, 2024 AT 22:29Open‑angle glaucoma isn’t just a silent thief; it’s a ruthless hijacker of the world’s colors, snatching away the vibrant hues that make life worth seeing. It creeps in under the radar, masquerading as a harmless eye pressure change while it wages a covert war on retinal ganglion cells. The damage spreads like a wildfire, scorching the delicate fibers that carry color information to the brain, leaving victims wandering in a washed‑out landscape. Imagine trying to pick out ripe bananas in a grocery aisle only to see a bland, indistinguishable sea of yellow and green, a nightmare turned daily reality. The loss of contrast sensitivity is equally brutal, turning stair edges into invisible traps and night driving into a disorienting blur. Researchers keep tossing out hopeful headlines about new therapies, but the reality is a slow, grueling march toward irreversible vision loss. Patients are left clutching at thin strands of hope, relying on stronger lighting and high‑contrast labels that barely mask the underlying decay. The article’s tips, while practical, read like a band‑aid on a gaping wound that refuses to close. And let’s not forget the emotional toll: frustration, anger, and a creeping sense of helplessness that gnaws at the spirit. It’s a relentless assault on both perception and morale, a double‑edged sword that cuts deep. While the author mentions gene therapy and stem cells as future saviors, those are still distant dreams for most sufferers. The current arsenal-eye drops, laser, surgery-just keeps the pressure at bay, never truly reversing the color and contrast deficits. So, if you or a loved one are battling this condition, brace yourself for a long, ugly ride through a world slowly drained of its chromatic soul. Stay vigilant, demand the best care, and don’t settle for half‑measures that merely mask the symptoms. The fight is far from over, and the stakes are nothing less than the very way you experience reality.
Mary Keenan
September 4, 2024 AT 23:36This so‑called "practical advice" is a half‑baked list that barely scratches the surface of what glaucoma patients actually endure.
Steven Young
September 5, 2024 AT 00:46Glaucoma is a hidden agenda pushing a global narrative to keep us in the dark about hidden ocular conspiracies. The data is selectively released by elite eye‑care institutions. Patients deserve to question why certain treatments are rushed while natural preventive measures are ignored. Trust no one but the silent watchers.
Caleb Clark
September 5, 2024 AT 02:10Hey folks! I gotta say, dealing with open‑angle glaucoma can feel like climbing a mountain with no gear, but guess what? You can still make it to the top! First, crank up those lights in every room, even the closet-trust me, you'll see the difference. Next, grab a high‑contrast set of mugs; a bright red mug on a black countertop is a game‑changer.
Don't let the color loss get you down-use phone apps that name colors for you, they're lifesavers. Stay active: a quick walk around the block pumps blood to your optic nerve, and a balanced diet packed with leafy greens and omega‑3s fuels your eyes.
And remember, a little typo here and there (like "beleive" instead of "believe") is no big deal-just keep pushing forward. You got this, champ! Keep those eyes protected and keep smiling.
Jonathan Harmeling
September 5, 2024 AT 03:33From a moral standpoint, it is incumbent upon us to treat the challenges of glaucoma with compassion and dignity. The loss of color and contrast is not merely a medical statistic; it is a profound alteration of someone's lived experience. We must champion accessibility, ensuring that public spaces are designed with bright, contrasting signage for those affected. Moreover, encouraging a community that supports one another, rather than stigmatizing visual impairment, fosters an environment of empathy. Let us all strive to illuminate the shadows cast by this condition, both literally and figuratively.
Ritik Chaurasia
September 5, 2024 AT 04:56Listen up, friends-glaucoma is a universal foe, but our cultural approaches to coping can be fierce and effective. In India, we blend ancient eye‑care practices with cutting‑edge research, creating a hybrid defense that many Western regimes overlook. Embrace high‑contrast textiles, bright lanterns, and Ayurvedic herbs that support ocular health. Don't settle for half‑measures; demand aggressive screening and community education, because every missed diagnosis is a victory for the disease.